Education Center
CISCRP creates easy-to-understand resources on clinical research. Explore our library of brochures, videos, medical hero stories, and more!
CISCRP creates easy-to-understand resources on clinical research. Explore our library of brochures, videos, medical hero stories, and more!
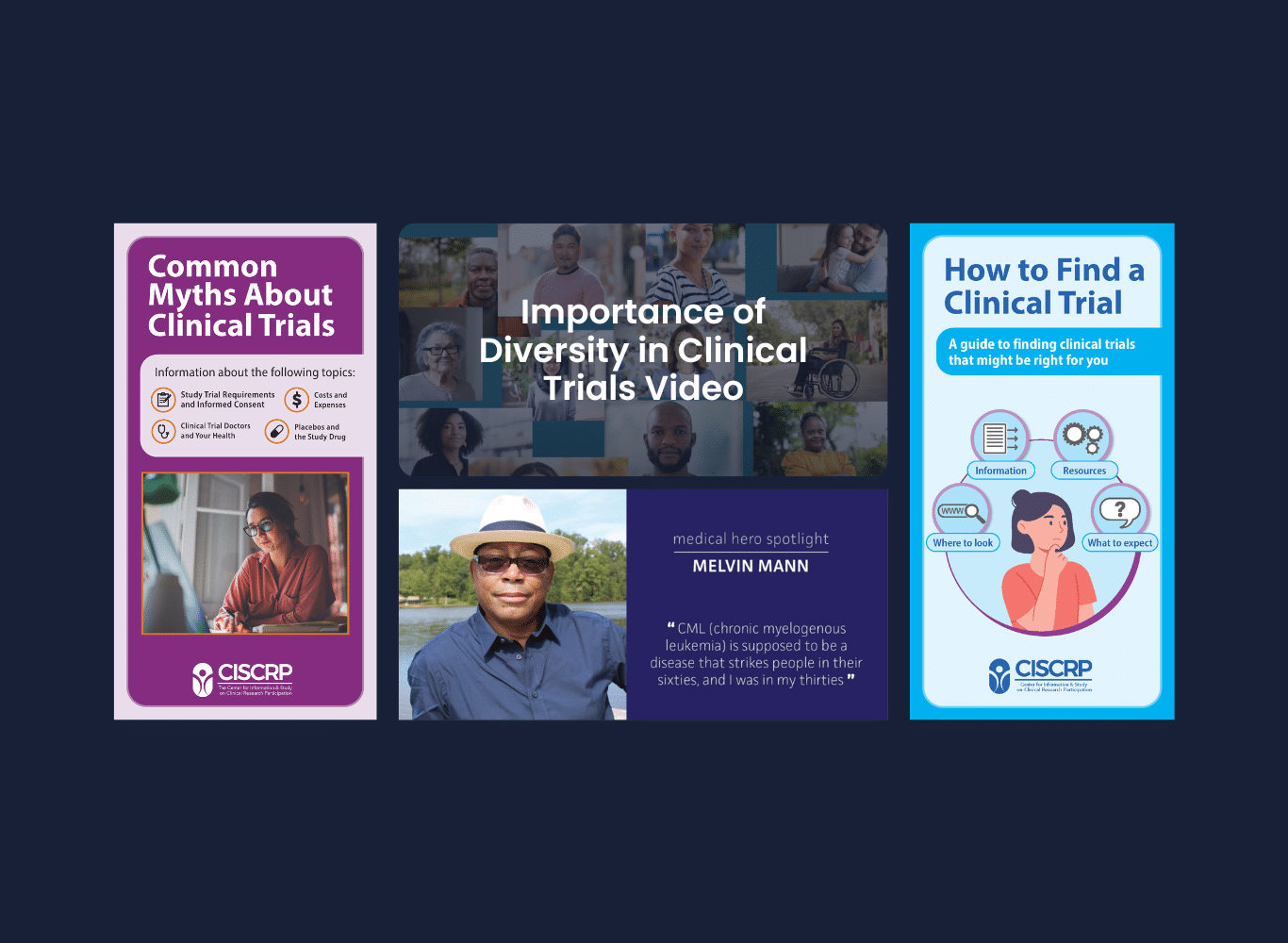
Our Finding Treatments Together brochures and award-winning videos provide information about clinical research and how it can impact you, your family, and your community.
It’s important to include participants of different age groups, from children to the elderly, in clinical trials to understand age-specific responses to treatments and medications. View our resources below on clinical research information for all age groups.

It’s important to shed light on the importance of including individuals with rare diseases in clinical trials, highlighting the challenges and how their participation can lead to breakthroughs in treatment.