Authored by Melissa E. Daley, Communications & Marketing Manager, CISCRP & Emma Kane, Senior Clinical Research Coordinator, Clinical Operations & Development, Sage Therapeutics
NOTE: CISCRP hosted a 2-part webinar series on postpartum depression (PPD), in collaboration with Sage Therapeutics, Inc. This is Part 1 of a 2-part article series, providing an overview of the first webinar, which focused on PPD, and shared perspectives from a PPD survivor, medical professionals, and a patient advocate. You can access Part 2 of this article series here (link to be created).
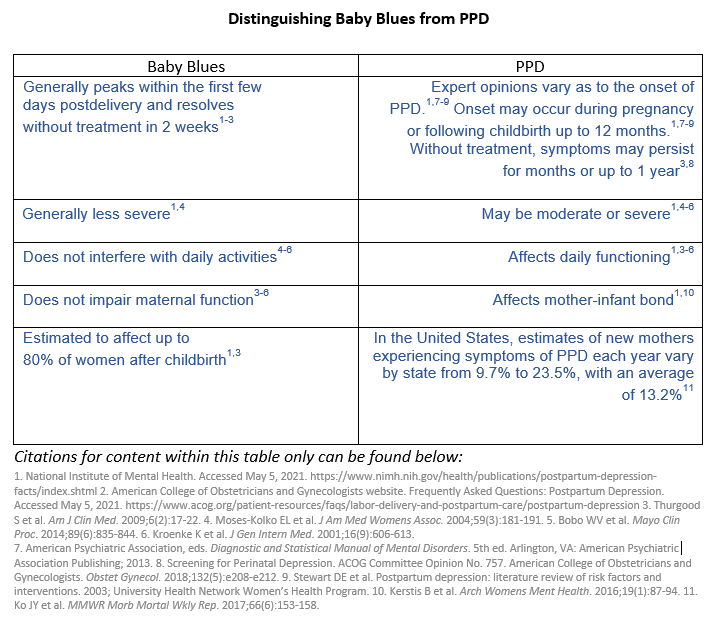
“I did not want to move. I did not want to breathe. And I did not want anyone to know,” explained Alexis, about her experience with postpartum depression (PPD). PPD is one of the most common medical complications during and after pregnancy[i]. PPD is more severe in scope than the “baby blues” that many mothers experience, which generally occur within the first few days of delivery and resolve without treatment in 2 weeks[ii].
Symptoms of PPD may vary, but can include:
- Changes in mood, including sadness, emptiness, hopelessness, irritability, persistent doubt, feeling overly anxious and thoughts of suicide
- Changes in the body including fatigue, difficulty sleeping or sleeping too much, aches and pains, and changes in appetite
- Changes such as trouble concentrating, remembering details or making decisions
- Social differences, such as withdrawing from family and friends, and distress or impaired ability to functional in social or work settings[iii]
“Clinically, we basically say that if someone has had an episode of depression during pregnancy or the postpartum year, we’re going to call it postpartum depression,” explains Dr. Constance Guille, Associate Professor, Department of Psychiatry & Behavior Sciences; Director of the Women’s Reproductive & Behavioral Health Program, MUSC. “Postpartum depression and baby blues are two very distinct entities.”
It’s estimated that about 50-80% of woman are affected by the “baby blues” after childbirth[iv].
“The symptoms are not severe, and they do not impact activities of functioning in any way,” explains Dr. Guille about the baby blues.
Alexis had an unexpectedly difficult delivery, but her daughter was healthy. From the outset, she had problems bonding with her baby. “I looked at her like I was holding an alien from another planet,” Alexis recalls. Initially, she blamed it on exhaustion, but it quickly became apparent to her that there was something more serious happening. With the support of her husband and parents, Alexis sought medical assistance. She ended up switching psychiatrists and medications many times, and nothing seemed to be working. Alexis voluntarily admitted herself to a psychiatric hospital where she remained for a month.
“At one point, I was sitting and waiting to see the doctor, when I overheard the social worker telling the counselor that I was faking it,” says Alexis. “I slid even further into the abyss. If they did not believe me, who would?”
After she left the hospital, her depression deepened.
“I struggled with thoughts of not wanting to be alive anymore,” says Alexis.
The stigma around experiencing PPD is real. However, there are healthcare providers who are working to change attitudes and perceptions around postpartum depression and individuals suffering with it. One approach adopted by medical professionals is to routinely ask about a patient’s mental wellness, both before and after delivery.
“You see a patient during her pregnancy about 20 times,” says Dr. Jason James, OBGYN, Private Practice in Miami. “For me to ask how she’s doing, how is she coping, is she feeling down or depressed, is she feeling anxious or guilty, all the kind of non-judgmental questions – if I ask it all the time and get lots of “No’s”, it normalizes the situation.” Routinely checking in with a patient about her mental health can reinforce her comfort level about transparently sharing any changes she may be experiencing.
“The more that people can share their stories, the more that other people can look at that person and say, ‘Oh gosh, I’m just like them!’, the better off we’ll be,” says Dr. Guille.
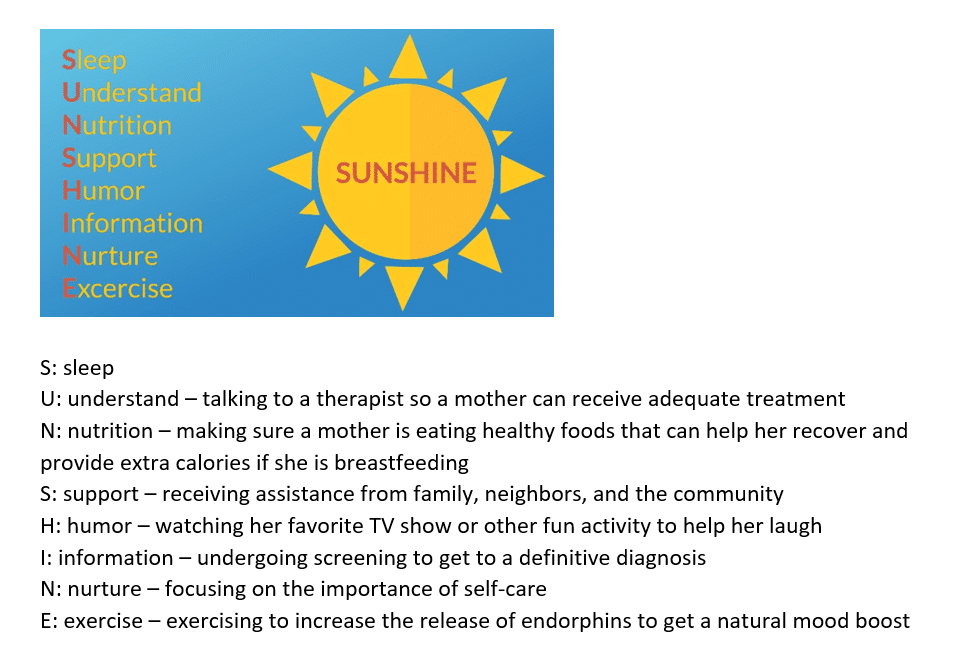
Providing a robust familial and social support system to postpartum mothers is key to assisting them in their recovery. “Having a baby is emotionally, psychologically, physically and financially depleting,” says Dr. Guille. Finding time to relax, getting enough sleep, and ensuring proper nutrition is essential.
Heather Dopp is a patient advocate and Mom Ambassador with 2020 Mom, a national organization with a mission to close gaps in maternal mental health care. She is a mother to two children. Her advocacy work is spurred by her own experience as a survivor of perinatal anxiety, depression, and suicidal ideation during her second pregnancy. Heather’s advocacy has taken her from the halls of the Utah State Capitol to the United States Capitol, with the purpose of improving awareness and increasing resources available to mothers facing maternal mental illness within the United States.
“From a non-clinical point of view, I have an acronym we like to use with maternal mental health. It’s SUNSHINE, and it’s a great way to remember the basic things you can help with for the mother struggling, so she can manage everything she is going through and hopefully try to thrive,” says Heather.
“For many women that I have talked to across the United States, we don’t know about postpartum and perinatal mental disorders in the first place. When it happens to us, we’re already experiencing ‘mom guilt’, and we don’t want to own up to it, because maybe we’re the only ones… we haven’t heard our friends talk about it, and we haven’t heard our providers mention anything about it.” says Heather.
Other patient barriers to discussing symptoms include:
- Mistrust and fear of being judged
- Lack of insurance coverage
- Time constraints
- Access to childcare during postpartum visits
- Lack of awareness regarding impact on own health and infant health
- Lack of information regarding where to seek treatmentv
Alexis changed physicians and treatments many times and took the time to do research and learn everything she could about PPD given there were very few medical professionals specializing in PPD in her location. Eventually, Alexis found a counselor and psychiatrist who supported her. They developed a treatment plan to best address her symptoms and over the next year, she was able to begin the healing process.
“I began to truly laugh and smile again. Life became brighter, more colorful and the darkness began to drift away,” Alexis recounts. Her daughter has no recollection of Alexis’ struggle with PPD, and they are very close.
Alexis says that PPD has taught her five important lessons:
- Never give up; postpartum depression doesn’t last forever.
- Don’t be embarrassed. Reach out and find a support system.
- Self-care is essential and it doesn’t have to cost money. It can be as simple as reading a book or taking a bubble bath.
- Do your best not to feel guilty.
- Tell your story, when the time is right, because it can help you heal, and also help others.
“I did not give up. I made it out of the darkness. And through the pain, I found a strength and courage that was always there, but needed some prompting to come out,” says Alexis.
To learn more about postpartum depression, access the webinar series, “Postpartum Depression & Being Informed” here. You can also access resources from Sage Therapeutics here and from 2020Mom here. Your healthcare provider should always be your primary source of information about diseases or disorders and treatment options. Please contact your healthcare provider with any questions pertaining to a medical condition.
ABOUT SAGE THERAPEUTICS
Sage Therapeutics is a biopharmaceutical company committed to developing novel therapies with the potential to transform the lives of people with debilitating disorders of the brain. We are pursuing new pathways with the goal of improving brain health, and our depression, neurology and neuropsychiatry franchise programs aim to change how brain disorders are thought about and treated. Our mission is to make medicines that matter so people can get better, sooner.
ABOUT CISCRP
CISCRP (Center for Information and Study on Clinical Research Participation) is a Boston-based, globally focused, non-profit 501(c)(3) organization providing public and patient education and advocacy. CISCRP’s mission is to inform patients and the public about clinical research and the important role that it plays in advancing public health and to help stakeholders in drug development engage with patients and the public as clinical research partners (www.CISCRP.org)
Sources:
[1] Ko JY et al. MMWR Morb Mortal Wkly Rep. 2017;66(6):153-158.; Martin JA et al. National Vital Statistics Reports; vol 68 no 13. Hyattsville, MD: National Center for Health Statistics. 2019.; DeSisto CL et al. Prev Chronic Dis. 2014;11:E10.; Centers for Disease Control and Prevention. Updated June 12, 2018. Accessed May 5, 2021 https://www.cdc.gov/reproductivehealth/maternalinfanthealth/diabetes-during-pregnancy.htm; Centers for Disease Control and Prevention. Updated February 28, 2019. Accessed May 5, 2021 https://www.cdc.gov/reproductivehealth/maternalinfanthealth/pregnancy-complications-data.htm; Roberts JM et al. American College of Obstetricians and Gynecologists Task Force on Hypertension in Pregnancy. Obstet Gynecol. 2013;122(5):1122-1131.; Callaghan WM et al. Am J Obstet Gynecol. 2010;202(4):353.e1-e6.[1] 1. National Institute of Mental Health. Accessed May 5, 2021. https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml; American College of Obstetricians and Gynecologists website. Frequently Asked Questions: Postpartum Depression. Accessed May 5, 2021. https://www.acog.org/patient-resources/faqs/labor-delivery-and-postpartum-care/postpartum-depression; Thurgood S et al. Am J Clin Med. 2009;6(2):17-22)[1] American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition. Arlington, VA: American Psychiatric Association, 2013.; National Institute of Mental Health. Accessed May 5, 2021 https://www.nimh.nih.gov/health/publications/postpartum-depression-facts/index.shtml)[1] Thurgood S et al. Am J Clin Med. 2009;6(2):17-22)v Prevatt BS et al. Matern Child Health J. 2018;22(1):120-129.; Byatt N et al. Arch Womens Ment Health. 2013;16:429-432.; Santora K et al. NIHCM Issue Brief. 2010. Accessed May 5, 2021 https://www.nihcm.org/pdf/FINAL_MaternalDepression6-7.pdf; Goodman JH. Birth. 2009;36(1):60-69.